A Brief History of Insulin
#dontfearthehypo
what is insulin?
Insulin is a hormone that is produced in the islets of Langerhans beta cells of the pancreas. A hormone is a chemical substance that is made in the body that controls or regulates the activity of certain cells or organs. Insulin acts to regulate blood glucose levels.
Did you know ?
- The islets of Langerhans cells were identified in 1869 by a medical student, called Paul Langerhans? He discovered small clusters of cells in the pancreas that looked different from their neighbouring cells when stained and viewed under the microscope but he did not know what they did.
- The pancreas has many jobs; it produces the hormones insulin, glucagon, amylin, somatostatin and pancreatic polypeptide. In addition to this it also produces digestive enzymes including trypsin, chymotrypsin, carboxypolypeptidase, pancreatic amylase, pancreatic lipase, cholesterol esterase and phospholipase; these digestive enzymes make it challenging for surgeons to transplant the pancreas.
- Another reason that we do not commonly see pancreas transplants happening in people with type 1 diabetes is that the immuno-therapy drugs that are required after transplant typically give a lower quality of life than you can achieve by taking insulin.
1901 - The function of the islet of langerhans
In 1901, thirty two years after Paul Langerhans discovered the islet cells, an American physiologist called Eugene Opie suggested that the islets of Langerhans cells produce insulin and that destroying these cells resulted in the symptoms of diabetes.
It was not yet clear exactly how insulin functioned. Later it became clear that insulin acts as a transporter allowing glucose to move from outside of the cell to the inside.
Did you know?
- Insulin is released by the pancreas and it goes into the blood stream.
- It travels throughout the body, although it does not cross into the brain.
- Insulin attaches to the surface of (almost) every single cell throughout the whole body so that it can help them move glucose (energy) from the blood to the inside of the cell.
- This allows our cells to get the energy they need to survive and work normally.
- It might help to think of insulin as a key that unlocks the door of a cell and allows glucose to get inside.
1916 - the race to treat diabetes is on
In 1916 Nicolae Paulescu worked on creating an extract from the pancreas of cows and was apparently successful in managing the symptoms of diabetes. He was called away to fight in World War 1 before he could publish his results. Paulescu’s extract was named pancreine, he later attempted to claim primacy when insulin was developed.
1920 - Struggling Surgeon is Inspired

On October 30 1920 a young Canadian surgeon, Dr Frederick Banting, was preparing to give a lecture to a group of medical students about the function of the pancreas. His preparations and reading inspired him to explore the idea that he might be able to isolate the secretions of the pancreas and produce an extract to treat diabetes. Banting shared his idea with John Macleod and they soon had a team of 4 people working to turn this idea into a reality.
On January 11 1922, Leonard Thompson became the first person with type 1 diabetes to receive an injection of insulin. Unfortunately Leonard had an allergic reaction to the first dose and James Collip worked day and night to improve the purification process and 12 days later Leonard received another injection, and this time it worked.
Did you know ?
The team that isolated and purified insulin was made up of four scientists working in London, Ontario.
Frederick Banting and John Macloed were awarded the 1923 Nobel Prize for physiology and medicine for this work. They shared the prize money with the other members of the team, Charles Best and James Collip. Banting and Macleod had an awkward professional relationship and looking at their history it seems incredible that they were able to set this aside, to some extent, and continue with the work to isolate insulin.
Nicholae Paulescu wrote to the Nobel prize committee to claim that his discovery of Pancreine in 1916 was first but without any published evidence the committee were unable to uphold his claim.
The team decided that insulin was too important a discovery to sell for profit so they sold the rights to Eli-Lilly for $1 each.
1 Unit of insulin was the amount of insulin required to give the rabbits in the original test laboratory a low blood glucose level (hypoglycaemia). This measurement of units of insulin remained in place until the 1980’s and until this time insulin was available in two strengths U40 and U80, providing 40 units or 80 units per cc, respectively, of insulin and it made calculating insulin doses very complex.
1930's; contaminating insulin on purpose
In the 1930’s Hans Christian Hagedorn became interested in contaminating insulin to modify the absorption rate. In its pure form the action of insulin is limited to a few hours.
Hans discovered that adding protamine (a protein from fish sperm) caused microscopic lumps to form in the insulin and gave the insulin a longer action profile, this had important therapeutic advantages. NPH insulin is one of the first examples of engineering drug delivery.
NPH insulin is named after Hans Christian Hagedorn the initials stand for Neutral Protamine Hagedorn.
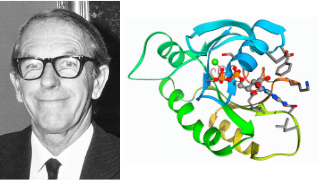
1958; another nobel prize for insulin
In 1958 Frederick Sanger won his first Nobel prize in chemistry for his work on sequencing the structure of proteins, especially that of insulin. This was the second Nobel prize related to insulin, the first of course was awarded to Banting and Macleod for developing insulin.
Sanger went on to win a 2nd Nobel prize for his contributions concerning the determination of base sequences in nucleic acids, which is important in understanding DNA (Deoxynucleic Acid).
1963 - 1978; Insulin is at the leading edge of genetic engineering

Personal Reflection I remember switching to human insulin at approximately the age of 11-12 years old, the change for me was remarkable. I no longer came up in huge hives at my injection sites. Some people had a difficult time when we switched to human insulin, it caused them to have more low blood glucose levels (hypos) and fewer symptoms of hypo.
Insulin is no stranger to being at the leading edge of technology and in 1963 it became the first protein to be synthesised in a laboratory.
This paved the way for synthetic human insulin using recombinant DNA to be produced by a company called Genentech and in 1978 the announcement of human insulin was celebrated as the most significant step forward in managing diabetes since insulin was discovered.
Around this time insulin was rebranded as human insulin and we moved away from U40 and U80 strengths to U100 insulin. The new scale of measuring a unit of insulin was no longer a legacy of those poor rabbits experiencing hypo’s back in 1921-1922.
1996; insulin analogues - what are they?
In 1996 Eli-Lilly launched the first insulin analogue under the name Lispro, but what is an insulin analogue?
In this sense analogue means comparable or similar to something else. The advantage is that the pharmaceutical companies can change the structure of the folds between the protein sheets to alter the action profile of insulin. This gives us access to faster acting insulin and insulin that has long durations of action. This was a breakthrough, now insulin is being produced that does not exist naturally.
Recombinant DNA insulin is still being produced and it works well for some people, it is used quite commonly in people with type 2 diabetes who need to start insulin therapy.

What is next?
The short answer is we just don’t know. Pharmaceutical companies invest fortunes into the development of new products and they are reluctant to share news until it comes to market.
JDRF, the type 1 diabetes charity, have been supporting research into smart insulin that switches on and off and automatically regulates blood glucose levels for quite a few years now.
In recent years, we have also been seeing developments in the bio-technology world to create cell lines of viable insulin producing cells. In addition to this, there is work ongoing to encapsulate these cells into semi-permeable membranes that can be implanted under the skin. The idea is to make these devices so that insulin is allowed to escape but the immune system can not attack the viable insulin producing cells inside the capsules.
We are also seeing some interesting work in the use of other drugs like SGLT2-Inhibitors. This class of drugs was developed for type 2 diabetes and has shown some, surprising and considerable, benefits in type 1 diabetes. Although some of these drugs like Dapagliflozin and Sotagliflozin have been licensed for use in type 1 diabetes many questions remain unanswered about them at this time and the licensing conditions restrict the use to a select group of people with type 1 diabetes.
If I am being honest, in over 40 years of living with type 1 diabetes I have seen many innovative products show promise and excitement and for one reason or another never quite reach the market place. I know that the pace of change and improvement is accelerating, I remain confident that things will only get better for people with type 1 diabetes. Who knows, the next leap forward might come from technology, insulin or a therapy that we use in addition to insulin?
topics that Might Also Help you...
Your diabetes may vary and that is OK – With Dr Alistair Lumb
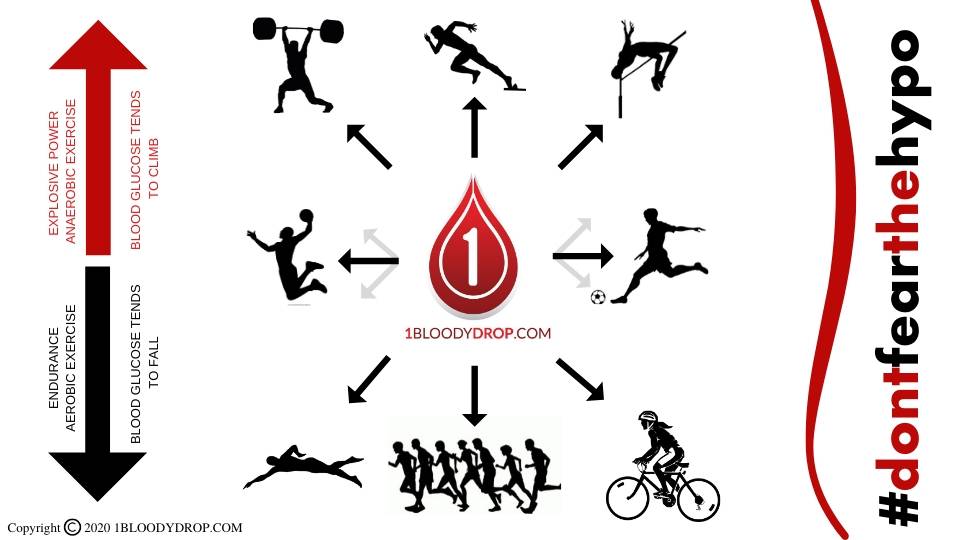
Managing my blood glucose levels during exercise – Pocket Medic